George Rappard, MD
NeuroInterventional Surgeon
What is Spinal Cord Stimulation?
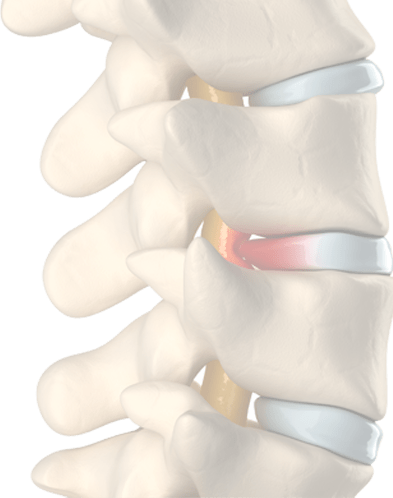
Spinal cord stimulation is one of the most complex and scientific subjects in all of spinal medicine. The basis behind spinal cord stimulation was the finding, in 1965, that transmission of pain signals traveling through the spine could be regulated by specialized nerve fibers in the back of the spinal cord. Soon after, in 1967, it was discovered that electrical stimulation in the back of the spinal cord could stimulate these specialized nerve fibers into regulating, or interrupting, pain signal transmission. As a result, the use of electrical stimulation of the spinal cord to treat chronic pain has grown. With that growth has come new techniques and technologies that now make this minimally invasive procedure more common than ever before.
Indications
As the use of spinal cord stimulation has grown, so have the indications. A common indication for spinal cord stimulation is failed back surgery syndrome, (or FBSS). In FBSS patients have undergone a prior form of surgery to treat spinal pain. Unfortunately, their pain did not resolve with surgery. Some of these patients may be given the option to have an alternative surgical procedure. In others, the cause of persistent or recurrent pain is not apparent. spinal cord stimulation provides an opportunity for long lasting relief in both groups. However, one must note that there are two types of FBSS patients; those with nerve symptoms and those with back pain symptoms. Back pain patients have traditionally been less successful at managing their symptoms with spinal cord stimulation. However, newer technologies are now resulting in better outcomes for FBSS whose symptoms are primarily back pain.
Arachnoiditis is another indication for spinal cord stimulation. Arachnoiditis is a term describing chronic inflammation of the nerve roots traveling up and down the spine. A layer of tissue enveloping the nerves, called the arachnoid layer, becomes inflamed. This inflammation in turn causes pain emanating from the nerve roots themselves. Primary Arachnoiditis is rare. Most cases are seen after spinal surgery and probably are best classified as a form of FBSS.
Complex regional pain syndrome (CRPS) is another indication for spinal cord stimulation.
CRPS is a condition where an injury to a nerve in or out of the spine results in a complex and painful syndrome, usually affecting a limb. Patients with CRPS suffer from a heightened and uncomfortable skin sensitivity, alterations in limb temperature, swelling, weakness, changes in skin and other uncomfortable signs and symptoms. It is common for CRPS patients to have a delayed diagnosis and to have tried many multiple injection procedures before being recommended for spinal cord stimulation. When a spinal cord stimulator is implanted, it is successful in most cases that have been properly selected.
Chronic neck pain and low back pain is a condition where pain has been persistent for at least 12 weeks. In the majority of cases, a careful analysis will determine the cause of chronic pain, called the “pain generator.” Injections, procedures or surgery can then be tailored to target the pain generator. Nonetheless, a portion of these patients are being offered spinal cord stimulation as a treatment option. It is important to note that there is little evidence to support the use of spinal cord stimulation as a final treatment option in chronic neck and back pain patients who have not tried another form of potentially definitive treatment. As a result, spinal cord stimulation is only indicated when there is no identifiable pain cause that can be addressed by surgery. If there is a surgically addressable cause, spinal cord stimulation is indicated only when the patient cannot tolerate the needed surgery.
spinal cord stimulation is only indicated when certain psychological conditions have been ruled out. These include severe cognitive impairment, poorly controlled or untreated addiction, social dysfunction or other disorders.
There are several other less common, but still important indications for spinal cord stimulation. Patients with vascular disease suffer from blockages to the arteries of the heart and limbs. Angina is a condition where heart blockages result in chest pain. When the blockages cannot be repaired, spinal cord stimulation is a treatment option for angina patients. Similarly, blockages in the leg can cause leg pain. This is called claudication. spinal cord stimulation may also be used as a means of treating claudication related pain.
Components

Every spinal cord stimulator has certain key components. The lead is the portion that is placed against the back of the spinal cord. Each lead consists of multiple electrodes. Each electrode has an anode and a cathode. Electrical current travels from the anode to the cathode. As many as 16 electrodes are present in needle placed leads (called cylindrical leads) and 32 in surgically placed leads (called paddle leads). The current amplitude flowing to each electrode can be switched on, off or adjusted. As a result, a greater number of electrodes in a lead allows physicians to alter the shape of the electrical stimulation field over the spinal cord in order to obtain the desired effect from stimulation.
The lead is connected to a generator. The generator is a power source that provides current and voltage to the electrodes in a lead via a connection. During a trial, or test of effectiveness, generators are connected to the implanted leads outside the body. After a successful trial, a new generator is implanted into the body and the connection with the leads is inside the body. For power, generators now come in rechargeable forms. This is advantageous because modern spinal cord stimulation systems require more power than before. Older systems would require an incision for removal and re-implantation of a freshly charged generator. Today, there is one generator system that can generate a current inside of an implanted lead without a physical connection. The generator is rechargabe and can be worn outside the body, like a pager. Unfortunately, this system is limited in the type of stimulation that it can provide.
The generator contains a program, telling the generator exactly how to administer the stimulation current. The program can govern voltage, current, the frequency of stimulation pulses, the amplitude and width of the stimulation pulses and whether the stimulation pulses are given in bursts or are constant.
Technique
Before being considered for spinal cord stimulation as a long-term treatment, a spinal cord stimulator trial is performed. The spinal cord stimulator trial is placed in a procedure room or operating room. In a trial, a physician places a lead delivery needle in the back. Through this needle a cylindrical lead, often referred to as a percutaneous lead, is placed. Using X-ray guidance, the physician advances the lead to the target location in the spinal cord. For low back pain the target is usually T8 or T9. For neck pain the target is usually C4 or C5. The needle is placed in the spine several segments below the target location.
After placing the lead and removing the needle the patient is left with a lead emanating from the skin of the back. The lead is then connected to a generator. At this point the physician, along with a technical expert, begin stimulation of the awake patient and adjust various stimulation parameters to see if there is adequate pain relief. As noted above, many different parameters can be altered while seeking optimal pain relief. This includes the number of electrodes activated and the current flow through those electrodes, the frequency of the stimulation pulse and width (in microseconds) of each pulse and the type of stimulation pulse. Multiple parameters will be adjusted in the operating room until adequate stimulation can be achieved. Sterile dressings are then applied and the patient returns to their normal activity to determine if pain relief is adequate. The trial phase typically lasts 3-10 days.
A spinal cord stimulation trial is considered successful if the patient has >50% drop in pain and improvement in functional abilities. At this point the patient is offered a permanent spinal cord stimulator implant. Like the trial, a spinal cord stimulator implant is performed in the operating room. The old trial lead is disconnected from the external generator. The old lead is then carefully removed. A small incision is then made in the back. If placing a cylindrical lead, a needle is then inserted into the spine and a new electrode is advanced to the target location. Leads with a greater number of electrodes are available but are too large to place through a needle. To place these leads a surgeon performs an opening in the back of the spine and manually inserts the leads.
The lead, placed through a skin incision, is then inserted and tunneled through the skin by puncturing the side of the incision. Meanwhile, an incision has been made over the back of the pelvis or lower abdomen and a small pocket has been surgically created for the implantable generator. The lead tunnels from the back wound, under the skin, and emerges inside the surgical pocket. The lead is connected to the generator. The incisions are then closed. Finally, the generator is programed, (this occurs externally, or outside the body), and spinal cord stimulation is begun.
Don’t Let Neck and Back Pain Ruin Your Life.
Minimally Invasive, State of the Art Technology.
contact us nowComplications, side effects and drawbacks
spinal cord stimulation implantation is a medical procedure and as a result carries similar complications as other procedures. One of these is infection, seen in 4.5% of cases. Infection is treated with antibiotics. If severe enough the generator or the lead may have to be removed.
Though rare, bleeding or inflammatory fluid can occur inside the pocket created for the generator. This can create significant discomfort and also raise the possibility of infection.
Pain at the site of the implanted generator is a common complaint, seen in 12% of cases. If not associated with infection or bleeding this generally becomes tolerable.
Device related problems are the most common issues seen in spinal cord stimulation. This usually takes the form of a broken lead, a lead that has moved from its original implantation site, (called a migrated lead), or a broken connection somewhere between the lead and the generator. Device related problems are seen in 38% of cases.
Overall, infections and device problems can result in device removal or revision. This can be seen in about 10%-12% of all cases undergoing spinal cord stimulator implantation.
Probably the most common side effect of spinal cord stimulation is called paresthesias. Paresthesias occur when the electrical stimulation of spinal cord nerve fibers causes a sensation of tingling, usually in the extremities. In the most traditional form of spinal cord stimulator, Paresthesia- spinal cord stimulator, paresthesias are sought after. Lead positions and electrical fields are adjusted until pain is replaced by paresthesias. In Paresthesia- spinal cord stimulation, the electrical pulses used in stimulation are tonic, meaning that they are continuous pulses in the 10-1,500 Hz (cycles per second) range. However, in some cases paresthesias may become bothersome. Today Paresthesia Free- spinal cord stimulation is available. In Burst Paresthesia Free- spinal cord stimulation, a burst of stimulation consisting of 5 pulses is delivered forty times per second. In High Frequency Paresthesia Free- spinal cord stimulation, an ultra-high frequency of 10 Khz (10,000 cycles per second) is delivered. Burst and High Frequency stimulation programs likely cause pain relief by novel methods not seen in Paresthesia- spinal cord stimulation.
One drawback to spinal cord stimulation is that patients may not be able to undergo MRI in the future. This is an important consideration given that patients being considered for spinal cord stimulation are more likely to require MRI than other types of patients. Because of this concern, some MRI compatible stimulators are currently available for use.
Alternatives to spinal cord stimulation
Most patients being referred for spinal cord stimulation have met the criteria of having severe pain and disability for over 6 months and having failed more conservative methods of care. However, there may be considerable variability in one of the most important indications; having no identifiable cause for pain that can be reasonably addressed with surgery. Some of this variability may come from the patient’s threshold for additional invasive procedures. If the only option being offered is a highly invasive procedure with an extended recovery period, a reasonable person may not want to pursue that. Additional variability may come from the physician side. Since there is considerable variability in what a physician might offer a patient, one physician’s patient may be considered as not having a surgically correctable problem while another physician’s patient with a similar problem may be considered surgically correctable.
Failed back surgery syndrome (FBSS) is one of the most common indications for spinal cord stimulation. In FBSS, a patient has had surgery and continues to have persistent pain. In most cases this can be resolved without the use of a spinal cord stimulator. To do so requires a persistent and detailed search to determine the patients “pain generator,” or actual cause of pain. This may require several diagnostic procedures to pinpoint one or more causes of pain.
One cause of FBSS is pathology in hard to access areas. Typical spinal surgical approaches have difficulty in reaching a portion of the spine referred to as “Mcnab’s Hidden Zone.” Unfortunately, up to 10% of herniated disc fragments may migrate into the hidden zone and can be missed at surgery. Endoscopic transforaminal spine surgery is a novel surgical approach that can easily reach the hidden zone, resolving pain without the lifetime use of a spinal cord stimulator.
Another cause of FBSS is simply that the problem that was surgically targeted was one of several problems, and not the only one. For example, in whiplash injury one might have a cervical disc injury and a cervical facet joint injury. Doing a disc replacement will fix the disc problem but there will still be joint pain with neck motion. These patients can benefit from cervical rhizotomy or cervical facet debridement after their disc replacements, performed at a surgery center with patients returning home the same day.
This may also be seen in the lumbar spine. A patient may undergo a successful lumbar discectomy to treat disc or nerve pain but find that they have residual pain of another pattern. A careful analysis may reveal a lumbar facet joint pain syndrome or a sacroiliac joint pain syndrome. These two syndromes can easily and successfully be treated with a lumbar or sacroiliac endoscopic rhizotomy, performed as a same day procedure.
Some forms of surgery may cause additional stress on adjacent spinal segments. For example, a fusion at L4/5 may place more stress on the L5/S1 disc because L5/S1 will have to overcompensate for the lack of motion at L4/5. This may result in early degeneration and disc pain at L5/S1. This is called a junctional disc syndrome. Renewed pain in this case is not because the original surgery failed. It’s due to a new condition at the adjacent spinal segment. In cases where the pain does not resolve with other means, endoscopic discectomy can address the new painful level as an out-patient procedure.
Importantly, patients should recognize that their physicians may not be offering them all their options in diagnosing the cause of persistent pain. This is not intentional but due to each physician’s unique experience and training, or one’s reliance on outside physicians for diagnosis before treatment. When options are given to patients, one should realize that in today’s day and age larger procedures have been miniaturized. What required an extensive recovery yesterday can now be done as an out-patient procedure. This is the case with all forms of endoscopic surgery. As a result, well informed patients have more options before going undergoing spinal cord stimulation.
Endoscopic spine surgery also has advantages to patients that will actually be undergoing spinal cord stimulation. Today, minimally invasive stimulator leads can be placed through a needle. These leads contain up to 16 electrodes. Larger leads are shaped like a paddle and may contain up to 32 electrodes, allowing wider variability in the spinal cord electric field generated. The implantation of paddle leads required an open surgery. Today, paddle electrodes can be placed in the spine through an endoscope requiring only an incision the size of a pinky nail. This allows patients to have the benefit of paddle leads without having to undergo larger surgeries.

